



When most people think about blood sugar problems, they imagine diabetes. But long before blood sugar crosses into the “diabetic” range, subtle changes are already occurring in how the body processes food and energy. These changes can be detected with advanced biomarkers — sometimes years before standard tests like fasting glucose pick them up .
At Longevity Health Clinic, we focus on identifying metabolic dysfunction early. Why? Because catching the problem upstream means we can often reverse the process before it leads to diabetes, heart disease, or accelerated aging.
Every time you eat, your digestive system breaks down food into glucose, fatty acids, and amino acids that enter the bloodstream. Glucose is the body’s preferred quick fuel, but it can’t get into most cells without insulin, a hormone produced by the pancreas. Insulin acts like a key, unlocking the door so glucose can enter muscle and fat cells for storage or use.
When the system works well:
But when the system is overloaded — particularly by excess calories, sugar, or highly processed foods — the body is forced to produce more and more insulin to achieve the same effect. Over time, cells stop responding as well. This condition is called insulin resistance .
Metabolic dysfunction doesn’t happen all at once. It progresses in stages, and different biomarkers change at different times. Based on large cohort studies, physiologic testing, and decades of OGTT data, here’s the typical sequence:
2-Hour Postprandial Insulin
Fasting Insulin and HOMA-IR
2-Hour Postprandial Glucose
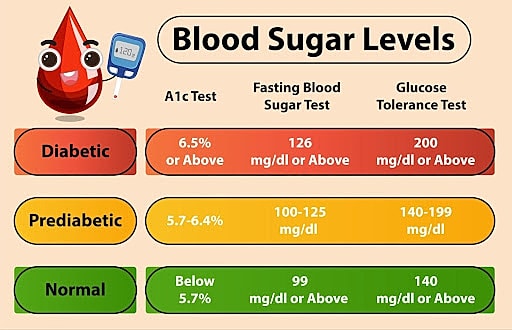
HbA1c (Hemoglobin A1c)
Fasting Glucose
Metabolic dysfunction doesn’t just affect blood sugar. It has ripple effects across nearly every system in the body:
The most exciting part is that insulin resistance and metabolic dysfunction are not destiny. With the right interventions, the process can be slowed, stopped, and even reversed.
1. An Anti-Inflammatory, Mediterranean-Style Diet
The Mediterranean diet — rich in vegetables, fruits, whole grains, legumes, lean proteins, olive oil, and omega-3 fish — consistently improves insulin sensitivity and reduces inflammation . High-fiber foods slow glucose absorption and blunt post-meal spikes.
2. Exercise
Both aerobic and resistance training improve insulin sensitivity. Aerobic activity helps muscle tissue take up glucose more efficiently, while resistance training builds lean mass — one of the strongest defenses against insulin resistance. Even a 10-minute walk after meals can meaningfully lower postprandial glucose .
3. Better Sleep
Sleep deprivation reduces insulin sensitivity within days. Patients who improve sleep duration and quality often see rapid improvements in fasting glucose, insulin, and HbA1c . Wearables like Oura or Whoop can make sleep tracking and habit change more tangible.
4. Reduced Stress
Chronic stress raises cortisol, which elevates blood sugar and worsens insulin resistance. Stress-management strategies — from breathing exercises to meditation or structured downtime — restore balance and lower metabolic strain .
5. Weight Loss (when appropriate)
Even modest weight loss (5–10% of body weight) can dramatically improve fasting insulin, HOMA-IR, HbA1c, and postprandial glucose. The key is targeting fat loss while maintaining muscle, something body composition analysis makes measurable.
6. Advanced Therapies: GLP-1 Medications
For patients who need additional support, GLP-1 receptor agonists (e.g., semaglutide, tirzepatide) can be transformative. These medications reduce appetite, slow gastric emptying, improve satiety, and enhance insulin sensitivity . Combined with lifestyle change, they help reset metabolic function while building long-term habits.
A 42-year-old patient came to clinic frustrated with creeping weight gain and fatigue. Standard labs from her primary care physician showed a “normal” fasting glucose of 90 mg/dL. But when we performed deeper testing:
We intervened with a Mediterranean-style diet, structured resistance training, and sleep optimization. Within three months, HOMA-IR normalized, and she lost fat while gaining lean muscle. She felt more energetic, and her long-term risk of diabetes decreased dramatically.
Metabolic dysfunction develops silently, often years before fasting glucose or HbA1c rise. The first warning sign is typically elevated post-meal insulin, followed by fasting insulin and/or HOMA-IR. Postprandial glucose rises next, then HbA1c, and finally fasting glucose.
If we wait until fasting glucose is abnormal, we’ve already lost years of opportunity to intervene. The good news is that metabolic dysfunction is one of the most treatable and reversible conditions in medicine.
At Longevity Health Clinic, we use advanced biomarker testing, continuous glucose monitoring, and personalized interventions to help patients move from early warning signs back to metabolic health.
References
Eckel RH, et al. “Insulin Resistance Syndrome.” Endocrine Reviews. 2005 – Review of systemic effects of insulin resistance .