



Osteoporosis is often described as an inevitable part of aging, but that perception is both outdated and harmful. Bone loss is not destiny. With the right combination of nutrition, strength training, hormone optimization, inflammation reduction, and targeted lifestyle interventions, it is absolutely possible to slow, stop, and even reverse bone loss—at any age.
At Longevity Health Clinic, we consider bone density a core longevity marker. Strong bones reflect strong muscles, balanced hormones, low inflammation, and resilient metabolic health. Understanding why osteoporosis occurs empowers you to take control of your long-term wellbeing.
This guide breaks down the root causes, early warning signs, health consequences, and the comprehensive strategies—well beyond medications—that protect and rebuild bone.
Bone is dynamic, living tissue. All day, every day, it undergoes remodeling: old bone is broken down (resorption) and new bone is formed (mineralization). Osteoporosis develops when bone breakdown consistently outpaces formation.
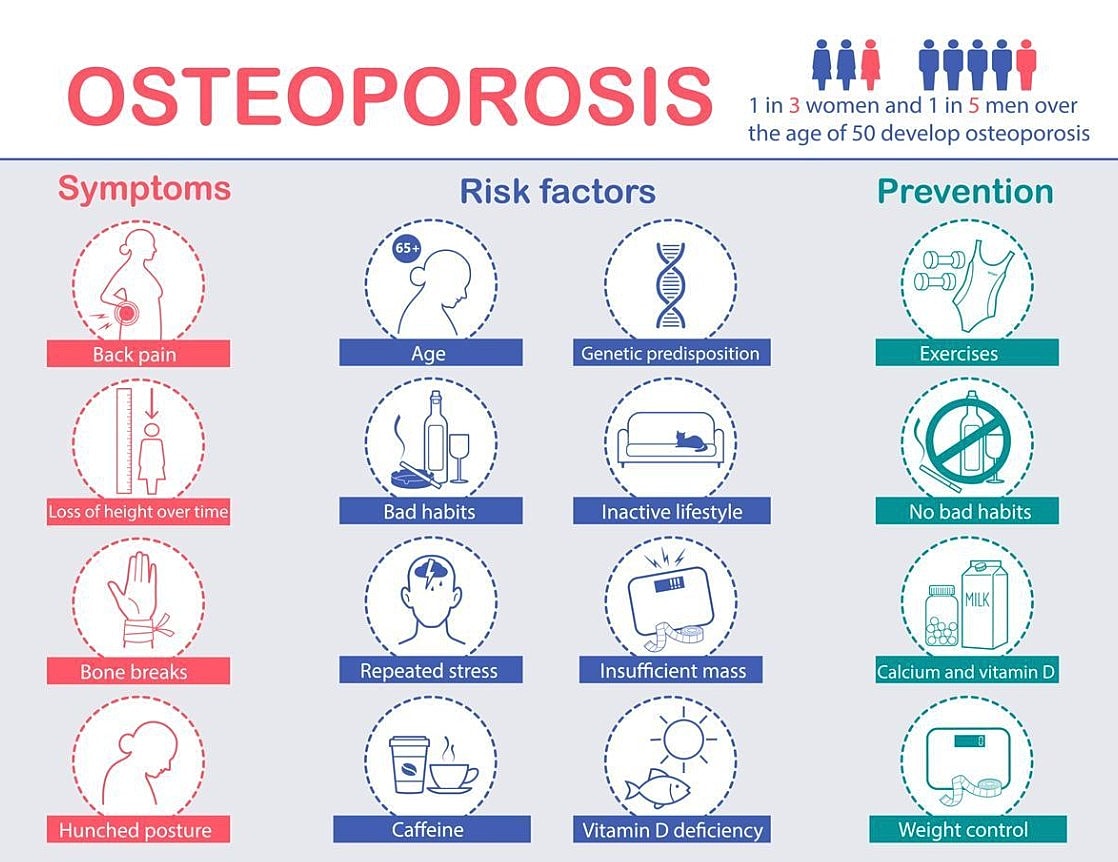
The major drivers include:
Estrogen is one of the most powerful bone-protective hormones in the body. After menopause, estradiol levels fall sharply, leading to:
This is why bone loss accelerates in the 5–10 years after menopause.
Inflammation drives bone loss by increasing osteoclast activity. Conditions such as chronic stress, insulin resistance, autoimmune disease, and poor diet all raise inflammatory load and accelerate bone breakdown.
Bone health is directly tied to metabolic and inflammatory health.
Bones require stress to stay strong. Without weight-bearing exercise or resistance training, the body down-regulates bone-building pathways. Prolonged sitting—common in modern life—is now recognized as a major risk factor for low bone density.
Bone formation requires protein, minerals (calcium, magnesium, potassium), and key vitamins (D and K2). Poor gut health reduces absorption of these nutrients and increases inflammation.
Low protein intake—especially common in women over 40—significantly weakens bone structure.
Thyroid dysfunction, parathyroid disorders, cortisol imbalance, and certain medications can all impair bone health.
Genetics set the baseline, but lifestyle determines whether your bones deteriorate quickly, gradually, or remain strong for decades.
Osteoporosis is often silent until a fracture occurs. Early clues may include:
DEXA scanning remains the gold standard for diagnosis.
Osteoporosis is not just a bone issue—it is a whole-body health issue.
Linked to loss of independence and increased mortality.
Cause chronic pain, height loss, and compromised lung capacity.
Often due to muscle weakness and impaired balance.
Low bone density is independently associated with higher all-cause mortality.
Medications can be useful, but lifestyle determines whether bone loss stops—or reverses. At Longevity Health Clinic, we focus on the interventions that modify bone physiology at the root.
Aim for 1.0–1.2 g/kg/day, or higher for active individuals. Protein stimulates IGF-1 and osteoblast activity.
Best sources include:
Food-based calcium is often better absorbed.
Optimal vitamin D levels (40–60 ng/mL) improve calcium absorption. K2 (MK-7) directs calcium into bone matrix where it belongs.
Essential for bone mineralization and vitamin D metabolism.
Emphasize:
Reduce:
A healthy gut improves mineral absorption and reduces inflammation.
Muscle pulls on bone, stimulating it to strengthen.
This kind of loading improves both bone density and bone architecture.
2–3 strength sessions per week can meaningfully improve BMD.
Preventing falls is as important as improving density.
Tools include:
Chronic cortisol elevation accelerates osteoclast activity.
Daily stress practices help:
Reducing stress improves nearly every aspect of bone physiology.
Most bone remodeling happens during deep sleep.
Improve sleep by:
Chemicals such as BPA, phthalates, and PFAS interfere with hormone signaling and bone metabolism.
Swap:
Hormone therapy, when used thoughtfully and safely, can be one of the most effective tools for protecting bone. This is especially important for women with low BMD or osteoporosis.
Clinical trials consistently show that estrogen therapy:
Estradiol works by decreasing bone turnover and improving calcium absorption. It is particularly effective when started within 10 years of menopause in low-risk women.
Progesterone receptors are present on osteoblasts, and laboratory studies show direct stimulation of bone-building pathways.
Evidence highlights:
At Longevity Health Clinic, we primarily use micronized progesterone for sleep, symptom management, and its synergistic support for bone formation.
Women produce more testosterone than estrogen pre-menopause, and androgen receptors are active in bone.
Research shows:
Testosterone helps maintain muscle mass, which further strengthens bone through mechanical loading.
Our clinical approach: We consider testosterone in selected, symptomatic women with documented low levels—often for energy, libido, and muscle support—with bone health as an additional benefit.
Medications such as bisphosphonates, denosumab, and osteoanabolic agents (teriparatide, abaloparatide, romosozumab) are appropriate for women with:
They work best when combined with strength training, optimized nutrition, and hormone balance.
Osteoporosis is not simply a loss of bone—it’s a reflection of hormonal shifts, metabolic health, movement patterns, nutrition status, inflammation levels, and stress resilience. By addressing these areas comprehensively, women can meaningfully improve bone density and reduce fracture risk.
At Longevity Health Clinic, we build personalized bone-strengthening plans rooted in lifestyle, supported by precision diagnostics and, when appropriate, evidence-based hormone therapy and medications. Strong bones are a direct investment in longevity, independence, and quality of life.